In this NewsFlash, how DNA sequencing identified an unsuspecting carrier of MRSA, why light at night makes mice depressed and a lonely rogue planet. Plus, a potential gene therapy cure for epilepsy...
In this episode

00:23 - Light at Night Can Harm Your Memory
Light at Night Can Harm Your Memory
Being exposed to bright lights at night could harm your health and your memory - even if you think you are sleeping normally...
Tara LeGates and her colleagues from John Hopkins University, Baltimore, exposed a group of mice to an alternating pattern of 3.5 hours of bright light followed by 3.5 hours of darkness over a 2 week period. This produced no change in their sleeping pattern, the overall length of time they slept for, or the levels of hormones that usually change at different times of the day.
But it did make the mice depressed, and reduced their abilities to form new memories. Depressed mice demonstrate behavioural signs, such as lower preference for sweet things. This can be an indicator of 'anhedonia'- the inability to feel pleasure, which is a symptom of depression in humans. Depressed mice also "give up" on certain tasks more readily, like poorly motivated people.
Humans with depression also often complain of memory problems. These mice were the same, establishing new memories less well than control animals.
This experiment meant that when the mice - which are normally nocturnal - were waking up to become active in what should be night-time, and dark, they were actually being exposed to light. And this - being exposed to light when the brain is not expecting it - the researchers think, is what made the mice depressed.
LeGates and colleagues, writing in the journal Nature, think that it's down to specialised light-detecting cells in the eye called intrinsically photosensitive retinal ganglion cells. These cells don't help animals to see but instead they detect when it is daytime or night-time, and they're used to set the brain's internal clock circuitry that enables animals to know when it's time to wake up or to go to sleep.
But, the researchers found, these cells also send signals to the parts of the brain concerned with mood and memory. And being exposed to light at the "wrong time" - so in the case of the mice, when they were awake and expecting it to be dark; for a human this would be the equivalent of working late at night in front of a bright computer screen - abnormally triggers these mood-related brain areas, causing depression, probably by provoking increasing the levels of the stress hormone cortisol.
Humans have the same light-sensitive cells as mice, so there is no reason to think that this couldn't apply to us. It is something important to bear in mind particularly for those who undertake shift- work, or regularly who work on computers late at night. So ignore your bed time and leave the lights on at your peril!
03:29.071 - A Rogue and Lonely Planet
A Rogue and Lonely Planet
A free-floating planet has been discovered in space...
08:13 - DNA Sequencing Stops MRSA Spread
DNA Sequencing Stops MRSA Spread
Professor Sharon Peacock, University of Cambridge
This week, the journal Lancet Infectious Diseases included a rather unusual detective story - one where rapid DNA sequencing was used in a hospital to track an outbreak of MRSA down to one unsuspecting carrier. It bears all the hallmarks of good television forensic crime drama, but it actually took place right here in Cambridge, and the research paper they released is said to be the first example of using this technique to bring an infection to a close.
Chris - The author of that study is Professor Sharon Peacock from Cambridge University. She's with us. Hello, Sharon.
Sharon - Hello, good evening.
Chris - Why did you do this?
Sharon - We want to control MRSA transmission, the passing of it from one patient to another, as much as possible because we want to contain any infections that might arise. And so, we need to see when MRSA does move from one person to another and we need to see it fast.
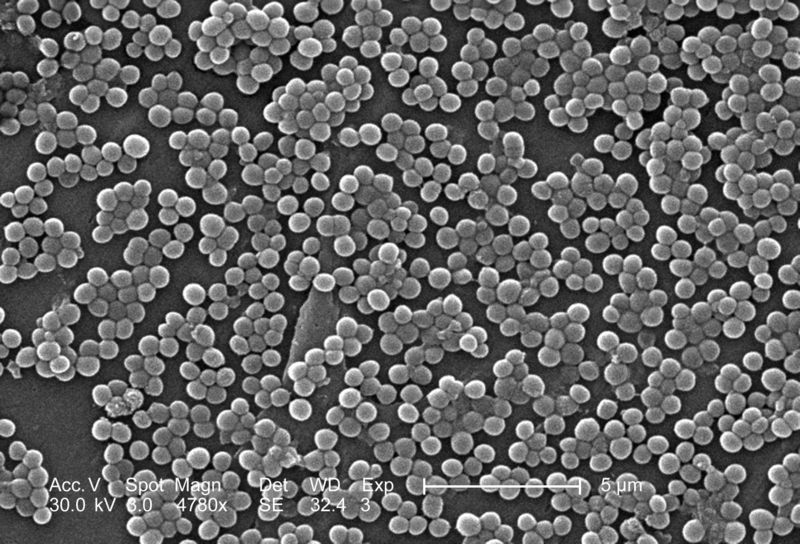 The way we do that at the moment is we work out whether two patients who are MRSA positive could've got it from each other because they're in the same ward at the same time. But what we can't do at the moment is to do any sort of typing on the bacteria to see how related the two are.
The way we do that at the moment is we work out whether two patients who are MRSA positive could've got it from each other because they're in the same ward at the same time. But what we can't do at the moment is to do any sort of typing on the bacteria to see how related the two are.
If we had a tool where we could see that they're were either related or unrelated, that would be very helpful because we could work out if transmission had occurred from patient A to patient B, but those tests aren't available at the moment and that's a problem for us.
Chris - So, we know that the two patients have got MRSA, but there's more than one form of MRSA, at a molecular level, so we don't know whether they've come into the hospital independently with their infection or something in the hospital is transmitting these infections between these individuals.
Sharon - That's exactly right. You can't see the transmission pathways between patients. So, what this new technology does is to actually sequence the whole genome with the bacterium.
Even just a few years ago, sequencing a bacterial genome would've cost hundreds of thousands of pounds and taken several years to do a single one. There's new technology now available which allows you to do sequencing of multiple genomes within a day actually, very, very fast and the price has actually fallen very rapidly. That means that we can bring this technology to clinical practice quite soon. In this research study, we really wanted to test out how useful that could actually be in trying to understand better an MRSA outbreak on our Special Care Baby Unit at Addenbrooke's Hospital.
Chris - Can you talk us through how you actually did the study? What were the steps and how did you investigate what was going on?
Sharon - Well, we had access to this technology and we knew that there was a suspected outbreak of MRSA on our Special Care Baby Unit, which should be investigated by our infection control team. Now, they were not sure whether an outbreak had occurred over an extended period of 6 months. There were cases coming into Special Care who were MRSA positive, but we weren't sure if they were related. And the reason for that is because throughout that 6 months, there were quite large gaps when there were no people who were MRSA positive at all. And so, one has to ask, how has that transmission gap been closed?
So, what we did in the first instance was, we took all of those isolates and we sequence them, and we're able to say very quickly that they were all so related at the genome level that this had to be an outbreak. At the same time we extended our search to look for bacteria that are coming from GPs actually in outpatient departments. We sequenced those and we found that actually, the outbreak was twice as big as originally thought and that there were cases actually in the community, people had developed infections. We really only linked that to the Special Care Baby Unit through the sequencing.
Chris - So that meant that you were then able to say right there, there are outbreaks occurring. How did you then go and find the individual that was causing those outbreaks?
Sharon - Well, having identified that there was definitely an outbreak, we put the Special Care Baby Unit under very close surveillance to see if new carriers or people infected with MRSA popped up. Actually, 2 months after the previous MRSA carrier, we found a new MRSA carrier, an infant, and we were puzzled by this because there's obviously a very long gap when we saw no MRSA at all. And it was at this point that we thought there must be a carrier amongst a member of staff.
And so, we gathered the staff together and got full agreement that they would be swabbed and we saw with 154 staff members, we found just 1 that was a carrier. And so, of course we immediately sequenced that and it was a direct match to the outbreak strain. What we think is that this person was involved in the outbreak. What that allowed us to do was to actually treat that individual so that the MRSA carriage is removed from them and that effectively stopped the outbreak from continuing any further.
Chris - How do you know that they gave it to the kids and not the other way around?
Sharon - I think that it will be difficult to be absolutely unequivocal about that individual causing spread throughout the entire outbreak, but what we did do with the staff carrier was we sequenced lots of single bacteria from their carriage population and we got genetic matches to before the 2-month gap and after the 2-month gap. We think that that is fairly strong evidence actually that that person was at least involved in that transmission event.
Chris - This is obviously extremely helpful in terms of guiding infection control strategies, but are there any other uses for this sort of technology in guiding how we tackle bugs of all kinds in the hospital?
Sharon - I think actually that there'll be numerous applications for this. We'll need to work out exactly where, when, and how to use it, but for example, it could be really key in investigating the food-borne outbreaks to work out if there is an outbreak and to help contain that. We could use it for example to get rapid drug susceptibility testing for people with tuberculosis. So, there is a very wide range of applications for this technology and I think that we will be seeing this brought into use in the next few years.

14:17 - Gene Therapy Cures Epilepsy
Gene Therapy Cures Epilepsy
Dr Stephanie Schorge, UCL
New research from University College London this week shows that gene therapy can potentially cure epilepsy in rats. Epilepsy affects around 50 million people worldwide. It’s a chronic disorder of the brain where patients can suffer seizures and loss of consciousness. These seizures are caused by out-of-control electrical activity in the brain. Dr Stephanie Schorge from University College London, co-author of this paper, published in Science Translational Medicine, explains why gene therapy was an attractive proposition...
Stephanie - Although we now have a set of drugs that can treat epilepsy, there is an incredibly large subset of patients that don’t respond to any of the drugs. In fact, there are people who have epilepsy with seizures that are recurring regularly and this is a risk of death. It’s roughly 1 in 100 per year so this is a life-threatening thing. One of the treatments is to remove the bit of brain that causes seizures. That’s not your first choice for treatment, but for some people, even removing the bit of the brain isn’t a great possibility because there are bits of your brain that you can't just cut out without stopping use of an arm or speech. So, for those people for whom drugs don’t work and you can't cut out the piece of brain because it’s so important, they have no choice but to live with these seizures. And so, we’re looking for a completely new approach to treating epilepsy and we decided to take this avenue of gene therapy. You can use genetically modified viruses to deliver little bits of DNA directly to neurons, only in that little piece of brain that is triggering the seizure and you express maybe one gene that just slows them down. It doesn’t silence them, it doesn’t turn them off, but it just stops them from triggering seizures.
Ben - So, what actually is the biological basis of epilepsy? What's happening in that part of the brain that then leads to what's been called an electrical storm throughout the rest of the brain?
Stephanie - That’s a fabulous question and I wish there was an answer. There's this theory that there's an imbalance between excitation and inhibition, and that generally speaking, you have more excitation than you want and less inhibition than you want. That means that excitation gets out of hand and you get the feedback, a buzz, a seizure, a storm, and the underlying genetics of that were really quite mysterious. But now, through these families who show up in clinic who will have epilepsy running very strongly in their family, in the last 10, 15 years, genes have been coming out and we’ve been learning from these patients that if you have a mutation that destroys one gene, that can lead to epilepsy. So our thought is, if we replace that gene or if we give more of that gene to those cells, maybe we can dampen epilepsy. And actually, the gene that we’re working with that we’re really, really most excited about, it’s from a boy who showed up in a clinic in Scotland a little more than a decade ago. He was 3 years old and his family had epilepsy. He had this very rare, only a dozen families in the world or so have this disease, and we went and looked in his family and sequenced the DNA and found a mutation of one gene called the Shaker Potassium Channel. It’s called the Shaker Potassium Channel because in Drosophila, the fruit fly, when you have a mutation in this gene, they shake. They have little epilepsy-like seizure things. Of course, they're flies so it’s hard to say it’s really epilepsy, but in this family, they had a mutation in this gene and they were also having seizures. The thing that this channel does, it’s a potassium channel. When a potassium channel opens, it allows positively charged potassium ions to leave the neuron and that makes the inside of the neuron relatively more negative and more negative neurons are less excitable, so maybe, less likely to trigger a seizure.
Ben - So, adding these potassium channels means that the nerves are less likely to fire off, so you're less likely to get this uncontrolled activity. How do you actually go about adding it?
Stephanie - We used a virus. It’s a virus that’s derived from HIV. All the bits that make HIV have been stripped out and instead, it’s been replaced with this Shaker Potassium Channel gene and we’re using a rat model of epilepsy that is like the human epilepsy. It’s really resistant to drugs and has a very sharp focus, a small area of the brain that is triggering the seizures and so, we’re injecting a tiny amount of virus into that exact tiny little focus. And when we first tried it, we were a little anxious because there's not that many neurons that are affected and we said, “Oh, it’s not going to be enough” but sure enough, after watching over a period of – it took about a week and a half. The seizures that were well-established in these animals just went away, and went away, and went away, and were effectively cured.
Ben - And once you’ve added this gene, is there any way to control its expression?
Stephanie - The viruses we use, once they go in, they seem to stay in. The gene that we chose is one that normally, when a cell is just sitting quietly, it’s not going to do anything. If somebody decides after 10 years that they want the gene out, the model that we used in this trial, you couldn’t do that. There are several other possible viruses that you can use that you could switch things on and off, but those are a little further downstream. We’re really interested in moving this to the clinical trials and doing pre-clinical trials, and all the challenges that lie therein. One advantage we think we have is that this is a human protein and it’s a human protein that normally occurs in human neurons. So we’re not adding something that isn’t there already. We’re just slightly changing the amount of something that’s there already in a very small subset of cells.










Comments
Add a comment